Facts about Covid-19
Updated: June 2020; Share on: Twitter / Facebook
Languages: CZ, DE, EN, EO, ES,
Fully referenced facts about Covid-19, provided by experts in the field, to help our readers make a realistic risk assessment. (Regular updates below)
“The only means to fight the plague is honesty.” (Albert Camus, 1947)
Overview
- According to the latest immunological and serological studies, the overall lethality of Covid-19 (IFR) is about 0.1% and thus in the range of a strong seasonal influenza (flu).
- In countries like the US, the UK, and also Sweden (without a lockdown), overall mortality since the beginning of the year is in the range of a strong influenza season; in countries like Germany, Austria and Switzerland, overall mortality is in the range of a mild influenza season.
- Even in global “hotspots”, the risk of death for the general population of school and working age is typically in the range of a daily car ride to work. The risk was initially overestimated because many people with only mild or no symptoms were not taken into account.
- Up to 80% of all test-positive persons remain symptom-free. Even among 70-79 year olds, about 60% remain symptom-free. Over 95% of all persons develop at most moderate symptoms.
- Up to 60% of all persons may already have a certain cellular background immunity to Covid19 due to contact with previous coronaviruses (i.e. common cold viruses).
- The median or average age of the deceased in most countries (including Italy) is over 80 years and only about 4% of the deceased had no serious preconditions. The age and risk profile of deaths thus essentially corresponds to normal mortality.
- In many countries, up to two thirds of all extra deaths occurred in nursing homes, which do not benefit from a general lockdown. Moreover, in many cases it is not clear whether these people really died from Covid19 or from weeks of extreme stress and isolation.
- Up to 30% of all additional deaths may have been caused not by Covid19, but by the effects of the lockdown, panic and fear. For example, the treatment of heart attacks and strokes decreased by up to 60% because many patients no longer dared to go to hospital.
- Even in so-called “Covid19 deaths” it is often not clear whether they died from or with coronavirus (i.e. from underlying diseases) or if they were counted as “presumed cases” and not tested at all. However, official figures usually do not reflect this distinction.
- Many media reports of young and healthy people dying from Covid19 turned out to be false: many of these young people either did not die from Covid19, they had already been seriously ill (e.g. from undiagnosed leukaemia), or they were in fact 109 instead of 9 years old. The claimed increase in Kawasaki disease in children also turned out to be false.
- Strong increases in regional mortality can occur if there is a collapse in the care of the elderly and sick as a result of infection or panic, or if there are additional risk factors such as severe air pollution. Questionable regulations for dealing with the deceased sometimes led to additional bottlenecks in funeral or cremation services.
- In countries such as Italy and Spain, and to some extent the UK and the US, hospital overloads due to strong flu waves are not unusual. Moreover, this year up to 15% of health care workers were put into quarantine, even if they developed no symptoms.
- The often shown exponential curves of “corona cases” are misleading, as the number of tests also increased exponentially. In most countries, the ratio of positive tests to tests overall (i.e. the positive rate) remained constant at 5% to 25% or increased only slightly. In many countries, the peak of the spread was already reached well before the lockdown.
- Countries without curfews and contact bans, such as Japan, South Korea, Belarus or Sweden, have not experienced a more negative course of events than other countries. Sweden was even praised by the WHO and now benefits from higher immunity compared to lockdown countries.
- The fear of a shortage of ventilators was unjustified. According to lung specialists, the invasive ventilation (intubation) of Covid19 patients, which is partly done out of fear of spreading the virus, is in fact often counterproductive and damaging to the lungs.
- Contrary to original assumptions, various studies have shown that there is no evidence of the virus spreading through aerosols (i.e. tiny particles floating in the air) or through smear infections (e.g. on door handles or smartphones). The main modes of transmission are direct contact and droplets produced when coughing or sneezing.
- There is also no scientific evidence for the effectiveness of face masks in healthy or asymptomatic
individuals. On the contrary, experts warn that such masks interfere with normal breathing and may become “germ carriers”. Leading doctors called them a “media hype” and “ridiculous”. - Many clinics in Europe and the US remained strongly underutilized or almost empty during the Covid19 peak and in some cases had to send staff home. Millions of surgeries and therapies were cancelled, including many cancer screenings and organ transplants.
- Several media were caught trying to dramatize the situation in hospitals, sometimes even with manipulative images and videos. In general, the unprofessional reporting of many media maximized fear and panic in the population.
- The virus test kits used internationally are prone to errors and can produce false positive and false negative results. Moreover, the official virus test was not clinically validated due to time pressure and may sometimes react positive to other coronaviruses.
- Numerous internationally renowned experts in the fields of virology, immunology and epidemiology consider the measures taken to be counterproductive and recommend rapid natural immunisation of the general population and protection of risk groups.
- At no time was there a medical reason for the closure of schools, as the risk of disease and transmission in children is extremely low. There is also no medical reason for small classes, masks or ‘social distancing’ rules in schools.
- The claim that only (severe) Covid-19 but not influenza may cause venous thrombosis and pulmonary (lung) embolism is not true, as it has been known for 50 years that severe influenza greatly increases the risk of thrombosis and embolism, too.
- Several medical experts described express coronavirus vaccines as unnecessary or even dangerous. Indeed, the vaccine against the so-called swine flu of 2009, for example, led to sometimes severe neurological damage and lawsuits in the millions. In the testing of new coronavirus vaccines, too, serious complications and fail
ures have already occurred. - A global influenza or corona pandemic can indeed extend over several seasons, but many studies of a “second wave” are based on very unrealistic assumptions, such as a constant risk of illness and death across all age groups.
- Several nurses, e.g. in New York City, described an oftentimes fatal medical mismanagement of Covid patients due to questionable financial incentives or inappropriate medical protocols.
- The number of people suffering from unemployment, depressions and domestic violence as a result of the measures has reached historic record values. Several experts predict that the measures will claim far more lives than the virus itself. According to the UN 1.6 billion people around the world are at immediate risk of losing their livelihood.
- NSA whistleblower Edward Snowden warned that the “corona crisis” will be used for the permanent expansion of global surveillance. Renowned virologist Pablo Goldschmidt spoke of a “global media terror” and “totalitarian measures”. Leading British virologist Professor John Oxford spoke of a “media epidemic”.
- More than 600 scientists have warned of an “unprecedented surveillance of society” through problematic apps for “contact tracing”. In some countries, such “contact tracing” is already carried out directly by the secret service. In several parts of the world, the population is already being monitored by drones and facing serious police overreach.
- A 2019 WHO study on public health measures against pandemic influenza found that from a medical perspective, “contact tracing” is “not recommended in any circumstances”. Nevertheless, contact tracing apps have already become partially mandatory in several countries.
See also:
- Studies on Covid-19 lethality (overview)
- Open Letter by Professor Sucharit Bhakdi
- European Mortality Monitoring (EuroMomo)
June 2020
A. General part
Studies of Covid-19 lethality
Stanford professor John Ioannidis published an overview of Covid-19 antibody studies. According to his analysis, the lethality of Covid19 (IFR) is below 0.16% in most countries and regions. Ioannidis found an upper limit of 0.40% for three hotspots.
In its latest report, the US health authority CDC reduced the Covid19 lethality (IFR) to 0.26% (best estimate). Even this value may still be seen as an upper limit, since the CDC conservatively assumes 35% asymptomatic cases, while most studies indicate 50 to 80% asymptomatic cases.
At the end of May, however, Swiss immunologists led by Professor Onur Boyman published what is probably the most important study on Covid19 lethality to date. This preprint study comes to the conclusion that the usual antibody tests that measure antibodies in the blood (IgG and IgM) can recognize at most one fifth of all Covid19 infections.
The reason for this discrepancy is that in most people the new coronavirus is already neutralized by antibodies on the mucous membrane (IgA) or by cellular immunity (T-cells). In most of these cases, no symptoms or only mild symptoms develop.
This means that the new coronavirus is probably much more common than previously thought and the lethality per infection is up to five times lower than previously assumed. The real lethality could thus be well below 0.1% and hence in the range of strong seasonal influenza.
In fact, several studies have now shown that up to 60% of all people already have a certain cellular immunity to Covid-19, which was acquired through contact with previous coronaviruses (common cold viruses). Children in particular often come into contact with such coronaviruses, which could help explain their insensitivity to Covid19.
The new Swiss study may also explain why antibody studies even in hotspots like New York or Madrid found infection rates of at most about 20%, as this would correspond to an actual rate of nearly 100%. In many regions, the actual prevalence might already be well over 50% and thus in the range of herd immunity.
Should the Swiss study be confirmed, the assessment of Oxford epidemiologist Prof. Sunetra Gupta would apply, who predicted early on that Covid-19 is very widespread and its lethality below 0.1%.
Despite the comparatively low lethality of Covid-19 (deaths per infection), the mortality (deaths per population) can still be increased regionally and in the short term if the virus spreads rapidly and reaches high risk groups, especially patients in nursing homes, as indeed happened in several hotspots (see below).
Due to its rather low lethality, Covid-19 falls at most into level 2 of the five-level pandemic plan developed by US health authorities. For this level, only the “voluntary isolation of sick people” is to be applied, while further measures such as face masks, school closings, distance rules, contact tracing, vaccinations and lockdowns of entire societies are not recommended.
Regarding contact tracing, a WHO study on influenza pandemics from 2019 also came to the conclusion that from a medical point of view this is “under no circumstances recommended”, since it is not expedient for easily communicable and generally mild respiratory diseases.
It is sometimes argued that the rather low lethality was not known at the beginning of the pandemic. This is not entirely true, as data from South Korea, the cruise ships and even from Italy already showed in March that the risk to the general population is rather low.
Many health authorities also knew this, as leaked emails from Denmark in mid-March show: “The Danish Health Authority continues to consider that Covid-19 cannot be described as a generally dangerous disease, as it does not have either a usually serious course or a high mortality rate.”
Some media nevertheless continue to calculate an allegedly much higher Covid19 lethality rate of sometimes over 1% by simply dividing deaths by “infections”, without taking into account the age and risk distribution, which is absolutely crucial especially for Covid19.
The latest data from the European mortality monitoring Euromomo shows that several countries such as France, Italy and Spain are already entering a below-average mortality. The reason for this is that the average age of Covid19 deaths was very high and fewer people than usual are now dying in this age group.
See also: Studies on Covid-19 lethality
 Example: Death rate per age group in Massachusetts, USA ( source )
Example: Death rate per age group in Massachusetts, USA ( source )
The role of nursing homes
Nursing homes played an absolute key role in the Covid 19 pandemic. In most countries, one to two thirds of all Covid19 deaths occurred in nursing homes, and up to 80% in Canada and some US states. Even in Sweden, which did not impose a lockdown, 75% of deaths occurred in nursing facilities.
It is all the more worrying that some authorities have obliged their nursing homes to admit Covid patients from the clinics, which has almost always resulted in numerous new infections and deaths. This happened in northern Italy, England and the heavily affected US states of New York, New Jersey and Pennsylvania.
It is also known from northern Italy that the widespread fear of the virus and the announced lockdown of the country led to the flight of the predominantly Eastern European nurses, which further accelerated the breakdown of elderly care.
In the United States, at least 42% of all Covid19 deaths are accounted for by 0.6% of the population living in nursing homes. Nursing homes require targeted protection and do not benefit from a general lockdown of society as a whole.
It is well known that even common corona viruses (cold viruses) can be very dangerous for people in nursing homes. Stanford professor John Ioannidis pointed out already in mid-March that coronaviruses may have a case mortality rate of up to 8% in nursing homes.
In addition, it is often not clear whether these people really died from Covid-19 or from weeks of stress and total isolation. For example, there were approximately 30,000 additional deaths in English nursing homes, but in only 10,000 cases, Covid19 is noted on the death certificate.
In April alone, around 10,000 additional dementia patients without corona infection died in England and Wales due to weeks of isolation. Investigations into the situation in nursing homes have been initiated or requested in several countries.
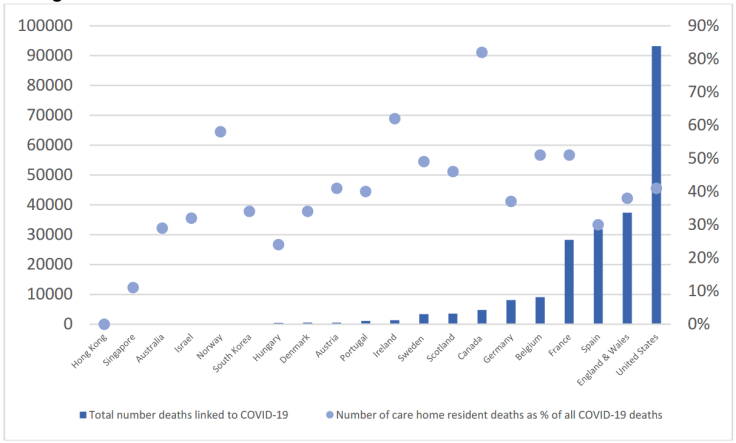
Nursing home deaths, absolute and percentage ( LTCCovid )
The role of hospitals
The second central factor regarding infections and deaths, in addition to the nursing homes, are the hospitals themselves. A case study in Wuhan already showed that around 41% of hospitalized Covid patients had in fact contracted Covid in the hospital itself.
Contagion in hospitals also played a decisive role in northern Italy, Spain, England and other regions that were severely affected, meaning that the clinics themselves became the main place of transmission of Covid19 to already weakened people (so-called nosocomial infection) – an issue that had already been observed during the SARS outbreak from 2003.
Based on current knowledge, those countries that managed to avoid outbreaks of infection in nursing homes and hospitals had comparatively few deaths. The general lockdown of society, however, played no role or even a counterproductive role (see below).
An additional factor is the sometimes fatal medical mistreatment of Covid patients with aggressive drugs or invasive ventilation, the risks of which experts have been warning about for months. In the US, for example, there have been questionable financial incentives to connect Covid patients to ventilators, a practice that is now being investigated in several states.
See also: An undercover nurse reporting from the ‘epicenter’ in New York City (Video)
The clinical picture of Covid-19
The well-known Hamburg medical examiner Professor Klaus Püschel presented his study (English) on the first 12 of 190 detailed corona autopsies at a press conference (German).
Professor Püschel again emphasized that Covid-19 “is not nearly as threatening as was initially suspected”. The danger was “too much influenced by media images”. The media had focused on severe individual cases and fueled panic with “completely wrong messages”. Covid-19 is not a “killer virus” and the call for new medicine or vaccines is “driven by fear, not facts.”
The specific cause of death of the examined cases was pneumonia, but in about 50% of the cases there were venous thrombosis in the legs, which can lead to fatal pulmonary embolism. The kidneys and heart muscle were also partially affected. Professor Püschel therefore recommends the preventive administration of blood-thinning medication for serious Covid cases.
With regard to thrombo
___
https://jamesfetzer.org/2020/06/swiss-research-report-facts-about-covid-19/